Haemorrhoids as a disease
- HAEMORRHOIDS are considered diseases of civilization of the 21st century
- The percentage of population suffers from haemorrhoids is still increasing
- MORE THAN 75% OF POPULATION FROM 25 YEARS suffers from haemorrhoids
What is it haemorrhoidal disease
 Problem with haemorrhoids may have many different causes: long standing or sitting, varicose veins, pregnancy, power and sedentary sports, problems with digestion and emptying (defecation), spicy food, fast food, obesity, genetic predisposition and, at all, current fast lifestile and stress. The veins are compressed for a long time, the blood flow is reduced in them and the blood is accumulated. Vein platelets in the anal area are opening enlarge and haemorrhoids develop.
HAEMORRHOID DISEASE BELONGS TO THE MOST WIDESPREAD DISEASES. MORE THAN 75 % OF POPULATION FROM 25 YEARS SUFFERS FROM HAEMORRHOIDS.
Problem with haemorrhoids may have many different causes: long standing or sitting, varicose veins, pregnancy, power and sedentary sports, problems with digestion and emptying (defecation), spicy food, fast food, obesity, genetic predisposition and, at all, current fast lifestile and stress. The veins are compressed for a long time, the blood flow is reduced in them and the blood is accumulated. Vein platelets in the anal area are opening enlarge and haemorrhoids develop.
HAEMORRHOID DISEASE BELONGS TO THE MOST WIDESPREAD DISEASES. MORE THAN 75 % OF POPULATION FROM 25 YEARS SUFFERS FROM HAEMORRHOIDS.
Causes of haemorrhoidal disease
Are more complicated and not yet exactly known. Some triggering factors have been confirmed:
- chronic constipation
- often diarrhea
- pregnancy, childbirdth
- sedentary employment
- some kind of sports (cycling, bending...)
- lack of physical activity
- frequent application of suppositories
- menstruation
- excessive alcohol consumption
- spicy food
- emocional factors, stress
- genetic prediction
Classification and symptomatology of haemorrhoids
Symptomatology of haemorrhoids
The common symptoms are:
- Bleeding after stool (light colored bleed on the toilet paper)
- Itching, burning
- Humidity, oozing
- Pain (from the beginning the feeling of blunt pressure)
Classification of haemorrhoids
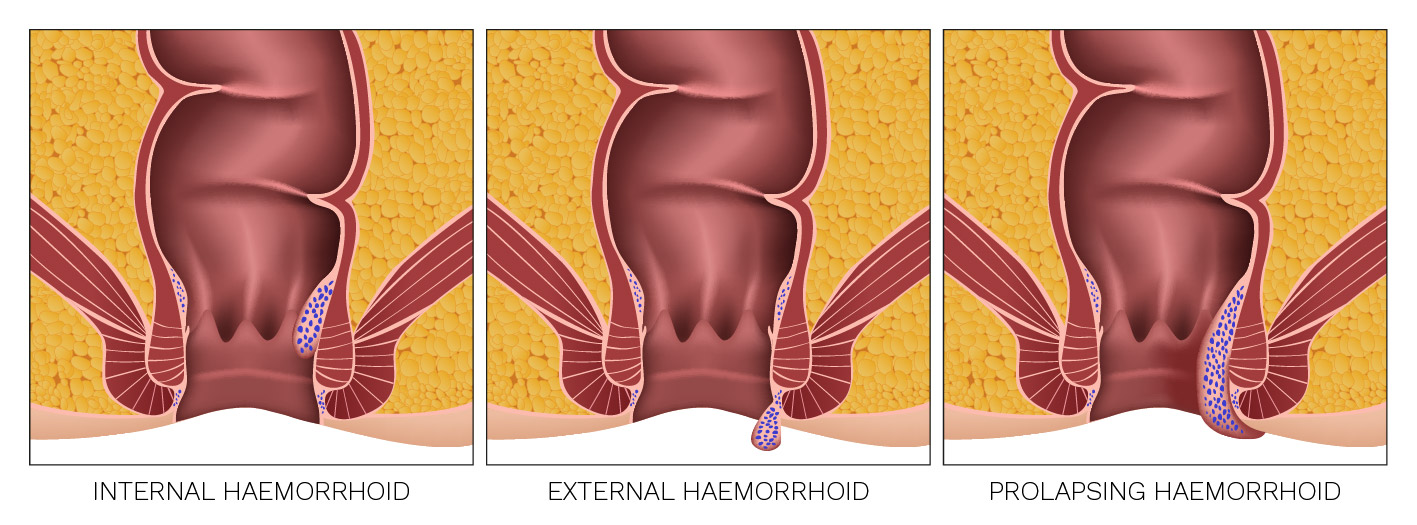
By occurence:
- Internal
- External
- Prolapsing
By extent:
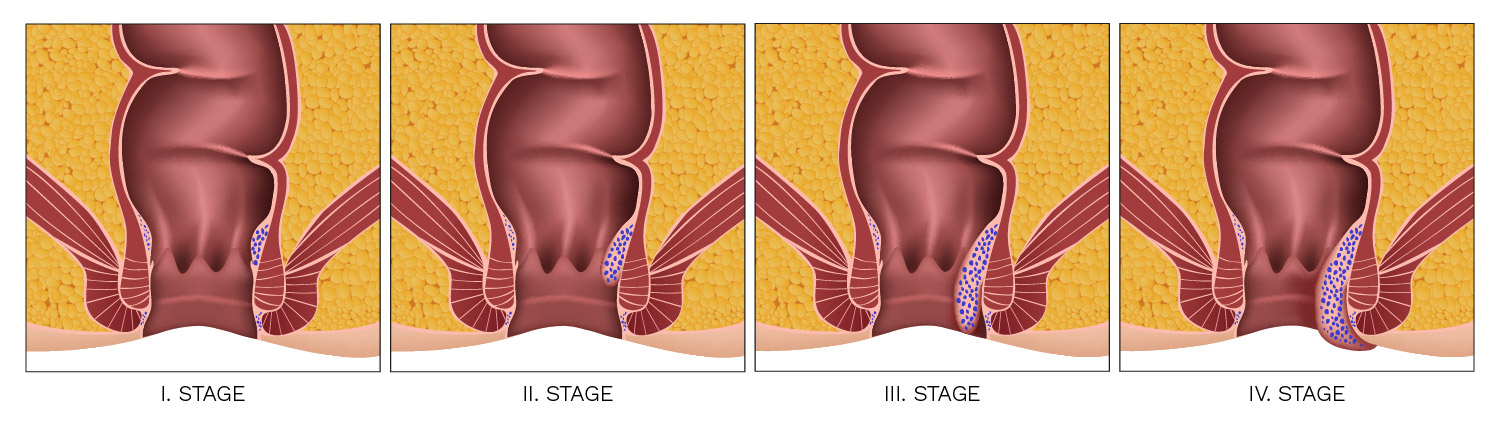
I.Stage
The veins are dilated, but only slightly, without any major problems. They manifest mostly just by light bleeding after a bowel movement, so that the patient observes traces of blood on a toilet paper.
II. Stage
Venous plexus prolapses into the anal canal (especially after emptying), but it reduces spontaneously, the presence of larger haemorrhoids is accompanied by itching, burning of anus and bleeding.
III. Stage
The symptoms are the same as in 2nd stage, the haemorrhoids prolapse upon defecation out of the rectum, but can be reduced manually.
IV. Stage
It is characterized by persistent difficulty – haemorrhoids of considerable dimensions permanently protruded from the anus, cannot be reduced. This vulnerable site of the patient often bleeds. Prolapsed mucosa itches, inflames and in an acute deterioration of the condition the patient experiences significant pain.
| Stage | Characteristic | Symptoms |
|---|---|---|
| I. Stage | Haemorrhoids without prolapse. There is no prolapse durring pressure on the stool, at defecation. | Bleeding |
| II. Stage | Prolapsing haemorrhoids that reduced spontaneously after defecation. | Prolapse, bleeding, discomfort |
| III. Stage | During pressure on the stool and during defecation, they break down from the anal canal – only manual reposition is possible. | Prolapse, bleeding, discomfort,pruritus |
| IV. Stage | Permanent prolapse without relation to defecation. It can not be | Prolaps, bleeding, reduced. pain, complications (ulceration, thrombosis, necrosis), signs of incontinence |
Rectum anatomy

Physiology of haemorrhoids
Haemorrhoids are normal anatomical structures that are a common part of rectum. Inner stitches form anal "pillows" that seal the anal canal, contribute about 15% to anus, 80% provide an inner anal sphincter.
Haemorrhoids and mucosal receptors are important in differentiating the character of intestinal content and are also helpful in maintaining of incontinence stool.
Character of intestinal content can be:
- gaseous
- liquid
- solid
Pathophysiology of haemorrhoids
Common mechanisms of haemorrhoids formation:
Mechanical theory
Predicts a gradual degeneration of haemorrhoids fixation in the context of increasing age which are released and become more mobile.
The “bristles” are no longer restricted by the ligament structures, they are expanded and consequently, with the increase of the intra-rectal pressure, the mucous membranes with loosened enlarged internal haemorrhoidal nodes are deflated. In the advanced phase of the disease, rupture of the supporting tissues and permanent prolapse of the internal hemorrhoids may occur.
Hemodynamic theory
Predicts a significant effect of direct arteriovenous shortness in the haemorrhoidal nodes leading to blood arterialization (oxygen supply of blood) in vascular extensions in submucosa.